A look at what ventriculomegaly means during pregnancy
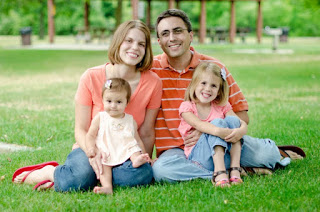
My oldest daughter just turned 5 years old. Megan is a bright, thoughtful, and creative little person who loves to be independent and continually amazes my husband and me. She also recently scored in the 99th percentile in an academic screening offered through our school district. We like to brag on her smarts, but we also know things could have turned out very differently.
Halfway through my pregnancy with Megan, she was diagnosed with fetal ventriculomegaly. The ventricles in her brain were slightly larger than normal. It’s a condition that occurs in about 1 in 1,000 births. By itself, the condition is not necessarily a problem. But it has the potential to develop into hydrocephalus, which puts pressure on brain tissue and can cause brain damage or require surgery at birth to prevent or lessen any further brain damage.
A specialist initially suggested I might want to terminate my pregnancy. It was a sad thought at the time, but it’s a sickening thought when I look at my healthy, intelligent 5-year-old and realize that a doctor once casually talked about ending her life.
All the worries began shortly after my ultrasound at 21 weeks. The ultrasound indicated Megan was healthy, but the technician couldn’t get her into a position to get a good view of her heart. We joked about the baby not cooperating and scheduled another ultrasound for the following week. I was pleased to get another view of the baby. When the second ultrasound was finished, the technician told me my doctor would “discuss it with me.” She sounded like she was holding something back, and it felt slightly ominous. A few minutes later, my doctor told me Megan’s brain ventricles were mildly enlarged. She referred me to a group of perinatal specialists at the hospital where I would be delivering.
“Your case is borderline,” my doctor assured me. “I’m sending you in just to be safe. They may look at you and ask why I even sent you in.”
I was fairly calm. I liked and trusted my doctor. She said she had delivered a baby years ago with the condition who was now a healthy patient in her practice. She told me not to worry, so I didn’t. At least not too much.
 |
|||||
| Megan at 21 weeks gestation, before the worries began. |
Around 23 weeks, I had my appointment in the hospital’s perinatal unit. I took the afternoon off work and went alone. The technician performed an ultrasound and then left me lying on my back on the table in a dim exam room while she fetched the doctor. I still had my pants pushed down around my hips with gel on my belly because the doctor would want to take a look himself. I waited for at least 30 minutes. I brought a book to read, but it was dark and I wasn’t in a comfortable position to do much reading. I grew worried and irritated.
The specialist, a man in his 40s, finally whisked in and glided the ultrasound device around on my belly for a few minutes. He asked if I knew why I was there that day. I explained in awkward, lay-person terms. The next few minutes blurred together as he said things like, “This kid could have brain damage,” and “In case you were wondering, you’re too far along in your pregnancy to terminate.”
“I wasn’t wondering,” I said.
“Do you want to speak with a genetic counselor?” he asked.
“Okay, I guess,” I said. “Do I need one? I really don’t know.”
A pretty young female genetic counselor with long blond hair sailed in and told me her name, handed me a business card, and disappeared. I thought counselors were supposed to be helpful, but I was not feeling reassured.
“You can also decide if you want an amniocentesis,” the doctor continued. “In the meantime, come back next week for a fetal echocardiogram.”
Somehow, I managed to wipe the goop off my belly, pull my pants up, and heft myself off the exam table. I felt numb as I drove home. Terms the doctor had thrown around like “brain damage” and “abortion” swirled through my head. I thought about amniocentesis, an invasive and sometimes miscarriage-inducing procedure. My husband, Josh, had just gotten home from work and was waiting to hear how things had gone. I told him the specialist was a jerk, and I cried.
I returned the following week for the fetal echocardiogram, and I had Josh come with me. I needed an extra set of ears and supportive arms. The echocardiogram was an elaborate term for an ultrasound that looked at the baby’s heart in greater detail. We were assured Megan looked healthy in every other way. There were no signs of Down Syndrome, mental retardation, heart defects, or other issues. She just had mildly enlarged brain ventricles. I saw the same specialist again, and he had the gall to repeat that I was too far along to terminate the pregnancy. My husband swiftly stepped in and affirmed our desire to carry the pregnancy to term. The doctor seemed to catch himself, and he paused to explain that where he had done his residency on the east coast, affluent couples chose to abort because of easily fixable conditions like cleft palates. How depressing, we told him.
 |
| Me at 37 weeks. |
We left the hospital that day feeling somewhat reassured because Megan’s condition seemed isolated. Still, I was instructed to come back every two weeks for the remainder of my pregnancy for ultrasounds to monitor the baby. Throughout the second half of my pregnancy, Megan’s ventricles measured around 11 millimeters, which is considered to be mild enlargement.
My mother-in law, a registered nurse who works in another department in the hospital, offered some of the best advice. “That’s not your baby,” she said. “It’s God’s.” More practically speaking, she’s a mother of four and recounted the major behavior problems she faced with one of her other sons, including run-ins with the law and jail time, and said she would welcome a child with special needs or another disability if she could choose between the two. I couldn’t argue with that logic. I took comfort. We prayed. Life went on and we coped with the ventriculomegaly diagnosis.
Two weeks later, I showed up for the first of many follow-up ultrasounds. My mother-in law showed up unexpectedly while I was in the waiting room. She had just gotten off her shift and asked if I wanted her company and support. It was a treat for her because she had never had an ultrasound herself and had never witnessed one.
I saw a different specialist that day, a friendly, bearded, middle-aged man with impeccable bedside manner. Megan’s ventriculomegaly was still the same. Her brain ventricles had not gotten smaller, but they also hadn’t grown larger. The specialist said he could not say it with certainty, but he thought Megan was going to be fine. He said the best place for her was in the womb, where she could continue to grow. They would watch and wait, and if it looked like she needed intervention, they would discuss options like a c-section. Yet, he was optimistic I would carry the pregnancy to term and deliver a completely healthy baby. My mother-in law, who has worked around doctors for decades and knows how to spot the good ones, was grinning and kept whispering to me to schedule the
rest of my ultrasounds with this doctor. That was the only time I was ever able to schedule with him. Apparently, he was popular with all the pregnant ladies. I started to relax more after that appointment, though.
My last ultrasound was around 36 weeks. Megan’s ventricles were still slightly enlarged. At that point, the bones in her skull were starting to fuse together and thicken, which was what they were supposed to do. As a result, though, it was getting harder to get a clear ultrasound image. The specialist I saw that day released me for the remainder of my pregnancy, with instructions to seek follow-up care for Megan after her birth.
 |
| Snuggling just hours after Megan’s birth. |
There always seemed to be a disconnect between the specialists and my OB’s office, though. My OB was antsy. She had been warning me for months that if Megan’s head grew bigger to accommodate the enlarged ventricles, simple physics would dictate the need for a c-section. Fair enough, I said, although I ended up not needing a
c-section. I was a week out from my due date when she asked if I wanted to be induced so we could “get this baby out” and check her head. I preferred to wait until after my due date to talk about induction, especially because the specialists were not in any hurry. Even after labor started naturally, four days before my due date, my OB insisted on speeding labor along by artificially breaking my water. I was clueless and consented. Almost immediately, labor
became more intense and painful. Now, I know better.
Oddly, there was no sense of urgency about Megan’s condition once she was born. I wasn’t too worried. Her routine checkup with a hospital pediatrician went well, but I self advocated and mentioned the condition to the baby nurse. Doctors performed an ultrasound on Megan’s head on the morning we were discharged. The baby nurse brought Megan back to my room explaining how she had washed her hair to get all the ultrasound goop off, and then we waited forever to hear the results of the ultrasound. I ordered lunch. We sat around. I nursed Megan. The nurse pestered and made phone calls and shook her head over how the doctors were taking their time.
“I think Megan’s just fine,” she said. “If there was a problem, you would have heard from the doctors by now.”
Finally, we received word that her head was perfectly fine. Her brain ventricles measured completely normal. Megan was in excellent health, and it was the culmination of months of worry, waiting, and prayer. I dressed Megan in a tiny purple sleeper, buckled her into her car seat, and we were escorted down to the hospital’s main entrance where Josh was waiting with the car. I was exhausted but elated as we drove home that afternoon to begin life as a family of three. Our daughter was perfect, and God was good.
I still continue to look at my oldest daughter in wonder, especially with that first specialist’s words still swirling in the back of my mind. “It’s too late to terminate,” he said.
 |
| A few days old and slightly jaundiced but otherwise perfect! |
I am glad terminating was not my first thought after receiving that uncertain initial diagnosis. About a week after her birth, when Josh and I were driving to the store to pick up a few things, with Megan snuggled in her car seat behind us, we both wondered aloud how many perfectly healthy babies are aborted because of scary, uncertain test results. Pregnancy hormones were still racing through my bloodstream, and I choked up as I said, “Look at Megan. She’s perfect.”
Let’s connect on social media:
Mumbling Mommy on Facebook
Mumbling Mommy on Instagram
Mumbling Mommy on Pinterest
Mumbling Mommy on Twitter
Category: Babies
Tags: abortion